Spirometry Introduction:
Spirometry is a valuable tool in occupational health — but it’s not the full picture when it comes to detecting work-related respiratory conditions.
At first glance, it might seem logical to assume that a normal spirometry test result means everything is fine. However, that’s not always the case. In fact, when workers report symptoms that suggest a possible occupational respiratory issue, a normal spirometry result doesn’t necessarily rule anything out — and further referral is often appropriate. Let’s explore why that is.
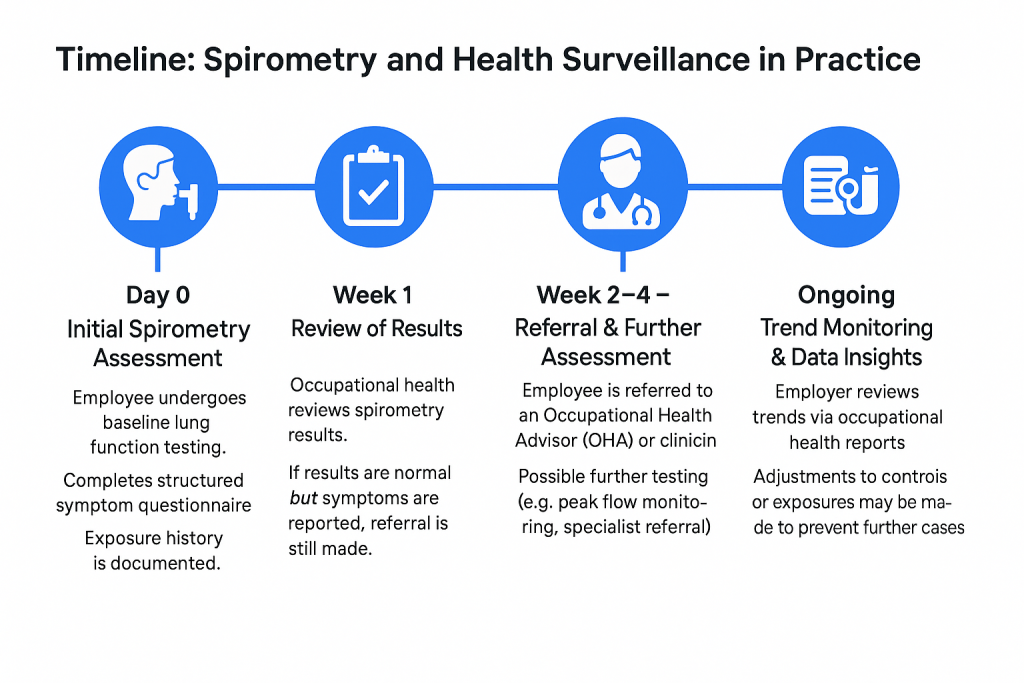
The Role of Spirometry in Health Surveillance
Spirometry is a simple, non-invasive lung function test that measures how much air a person can exhale, and how quickly. In occupational health, it’s used as part of routine health surveillance, especially in workplaces where employees are exposed to respiratory hazards like dusts, fumes, or sensitising chemicals.
The benefits of spirometry include:
- Establishing a baseline for future comparisons
- Detecting underlying conditions like undiagnosed asthma or COPD
- Monitoring changes over time when repeated periodically
- Supporting clinical decisions when combined with other information, such as symptom reports and exposure history
However, spirometry alone isn’t enough to detect all occupational respiratory diseases — particularly in the early stages.
Why Normal Spirometry Doesn’t Always Mean “No Problem”
One of the key limitations of spirometry is that many occupational respiratory conditions — especially occupational asthma — are episodic. That means symptoms come and go, often triggered by specific exposures in the workplace.
If a spirometry test is conducted when the worker isn’t actively experiencing symptoms, the results may appear completely normal. This can create a false sense of reassurance — for both the employee and the employer.
That’s why symptom questionnaires are just as important as spirometry, if not more so, in certain situations.
The Faculty of Occupational Medicine (FOM) provides clear guidance on this point:
“In many cases, especially for respiratory sensitisers, structured symptom questionnaires are the most sensitive method of detecting early disease.”
When a worker reports symptoms such as coughing, wheezing, or shortness of breath that appear to be work-related — even if their spirometry is normal — a referral for further clinical assessment is still the right course of action.
Common Questions: “Then Why Do Spirometry At All?”
It’s a fair question. If spirometry isn’t always reliable for detecting early signs of work-related illness, why include it in health surveillance at all?
The answer is that spirometry is still a valuable tool, just not a standalone one. Its value lies in how it complements other elements of health surveillance, particularly symptom reporting and exposure history.
For example:
- It helps detect non-occupational respiratory conditions that might still impact work
- It allows clinicians to track lung function over time and spot deteriorating trends
- It provides additional data points to support or rule out certain diagnoses
In short, spirometry plays a key role — but it must be interpreted in context.
Understanding Referral Decisions
When a referral is made following spirometry, it’s not necessarily because of the test result alone. In many cases, it’s the reported symptoms that trigger the referral — because they may indicate an underlying issue that needs further investigation.
This is standard clinical practice, and it aligns with both national guidance and long-standing protocols across the occupational health sector.
Takeaway: Don’t Rely on Spirometry Alone
Work-related respiratory illness can be complex and difficult to catch early. That’s why a multi-layered approach to health surveillance is essential. Spirometry is an important part of that approach — but the real insight often comes from listening to what workers report about their symptoms and experiences.
Employers should be cautious about interpreting a normal spirometry result as a clean bill of health. And workers should be encouraged to report symptoms without fear that “nothing will be done” if their test results are fine.
Final Thought:
Good occupational health practice doesn’t rely on just one piece of data. It combines clinical testing, structured symptom assessment, and knowledge of workplace exposures to protect workers and ensure any emerging issues are caught early.
If you’re an employer or safety professional looking to better understand how spirometry fits into your health surveillance strategy, reach out to an occupational health provider for tailored advice.
Request a Quote







